There’s a growing body of research investigating gut microbiota - the community of bacteria living in the gut - and immune responses and outcomes. As such, we’re getting a better understanding of the benefits of modulating gut microbiota when managing Cow’s Milk Allergy (CMA), sometimes known as Cow’s Milk Protein Allergy (CMPA), in formula fed infants.
What are synbiotics?
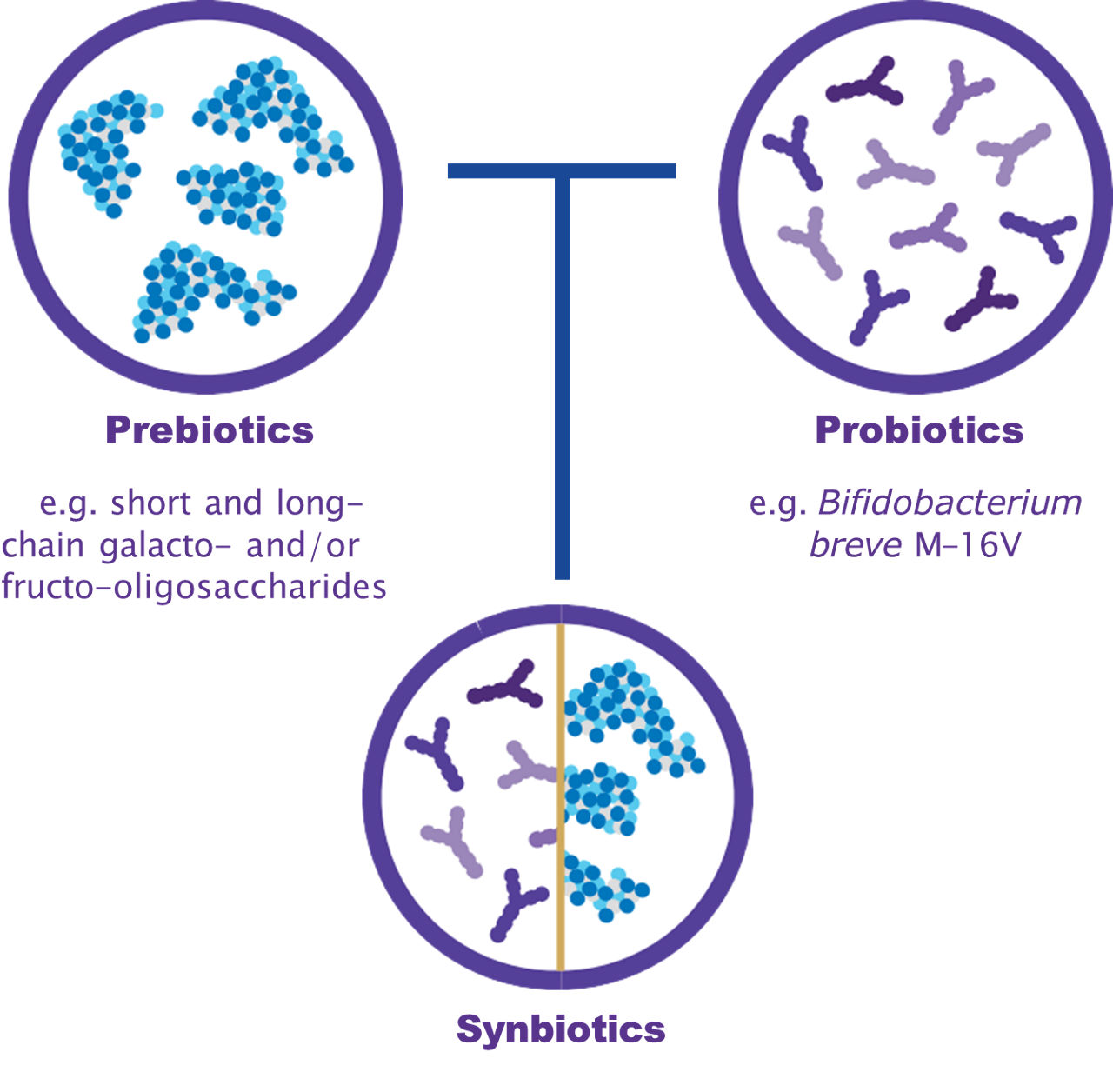
Synbiotics are a combination of prebiotics and probiotics1-2. Whilst it can be easy to confuse the two, they in fact have very distinct functions.
Prebiotics are a non-digestible food ingredient that stimulate the growth or activity of beneficial gut bacteria3. A probiotic on the other hand, is a type of beneficial bacteria that can help to rebalance gut microbiota4-5 when consumed in the right amount.
The objective of combining pre- and probiotics is to achieve stronger positive effects than with either component alone so that they are working synergistically6.
Gut microbiota and immune system development
With between 70-80% of immune cells residing in the gut7, the gut microbiota and immune system function are inextricably linked.
From the moment we’re born, gut microbiota play a very important role when it comes to immune system development and its responses8-9. At birth, the gut is essentially sterile, and isn’t yet populated with the variety of bacteria needed to form an effective microbiome6. Following birth, microbiota start to become established, with further diversification when weaning onto solid food and a process that continues to change over time. The intestinal microbiota is fully matured by about three years of age8-9. The immune system itself can also be described as immature at the time of birth; evolving and adapting as we grow and learning to distinguish between those things that are a threat and the things that are beneficial.
Working together, gut microbiota and the immune system play an essential role in defending against harmful pathogens, maintaining tolerance of antigens10, and strengthening the body’s immune defences11.
For infants and children, it’s especially important to maintain the balance between the gut microbiota and the immune system given its role and influence in shaping life-long health12.
What causes gut dysbiosis?
Gut dysbiosis occurs when there’s an imbalance in the body’s gut microbiota13. Gut dysbiosis is associated with several diseases, including inflammatory bowel disease, obesity, type one diabetes and allergic disorders14-15.
There are several factors that can influence gut dysbiosis, including diet, the use of antibiotics, complementary feeding and physical and psychological stress16. However, the first weeks and months of life can also have a huge impact on the health of gut microbiota, with particular risk factors being17-18:
● Premature birth
● Birth by caesarean
● Antibiotics
Microbiome and allergies: the impact of gut microbiota dysbiosis on health and the development of Cow’s Milk Allergy
Healthy breast-fed infants typically have a higher amount of the probiotic Bifidobacteria than other species. This probiotic is transmitted via birth and through breast milk19-20. Breast milk also contains non-digestible oligosaccharides, a type of complex carbohydrate that’s readily consumed by Bifidobacteria21.
Infants who are allergic to cow’s milk often present with gut dysbiosis, having an altered profile of gut microbes characterised by much lower levels of Bifidobacteria, and higher levels of adult-like bacteria22-23.
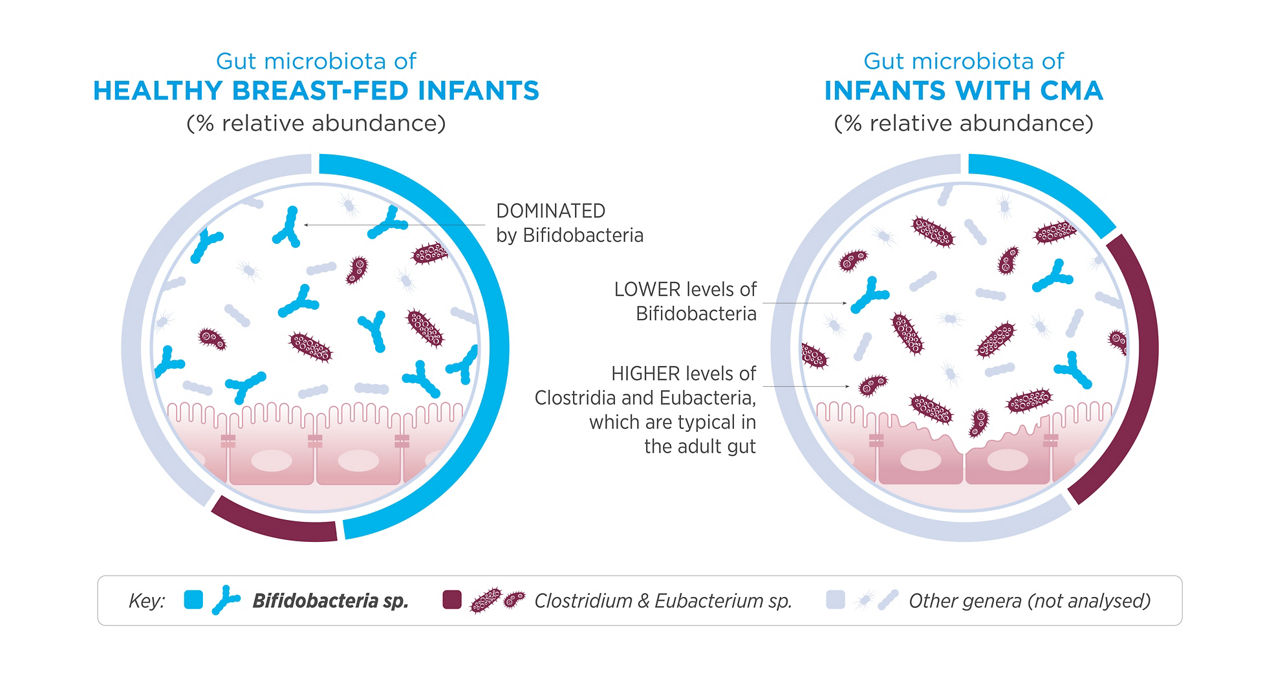
This imbalance of microbiota caused by gut dysbiosis can trigger an abnormal immune response, which in turn can contribute to the development of a food allergy, for example, a Cow’s Milk Allergy15, 22.
Synbiotics and the management of Cow’s Milk Allergy
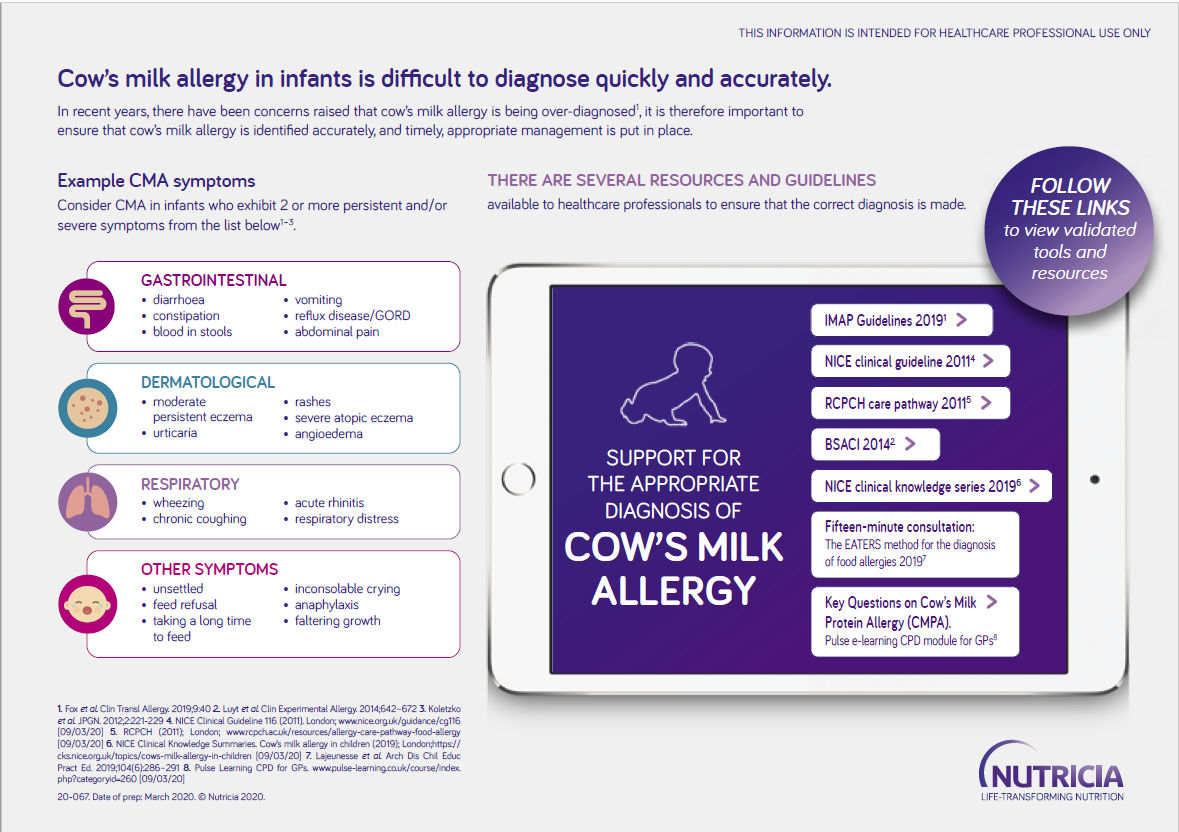
A Cow’s Milk Allergy occurs when the immune system has an abnormal reaction to cow’s milk protein26. Typically developing during the first few months of an infant’s life, Cow's Milk Allergy affects around 2-5% of infants under the age of one27.
Some studies have shown that synbiotics could help to regulate microbiota and immune response, both directly and indirectly24. They can be of assistance when it comes to managing, and reducing the severity of, symptoms of a Cow's Milk Allergy25, 29.
Future of Cow’s Milk Allergy management
Currently, the main management for a Cow’s Milk Allergy is to remove all sources of cow’s milk from an infant’s diet. In the case of breastfed infants, the mother will usually be advised to follow a dairy-free diet to avoid cow’s milk passing through breast milk27-28.
Although this approach is effective in managing Cow’s Milk Allergy symptoms, synbiotics could in the future play an important role here. Synbiotics can help to rebalance and repopulate the gut microbiota with healthy bacteria, targeting the source of gut dysbiosis and therefore potentially the programming and development of immune responses and allergy1.
- Fox A, et al. World Allergy Organ J. 2019;12(5):100034.
- Swanson KS, et al. The International Scientific Association for Probiotics and Prebiotics (ISAPP) consensus statement on the definition and scope of synbiotics. Nat Rev Gastroenterol Hepatol. 2020;17(11):687-701
- Gibson GR, et al. Expert consensus document: The International Scientific Association for Probiotics and Prebiotics (ISAPP) consensus statement on the definition and scope of prebiotics. Nat Rev Gastroenterol Hepatol. 2017;14(8):491-502. doi:10.1038/nrgastro.2017.75.
- Hill CF, et al. "The International Scientific Association for Probiotics and Prebiotics Consensus Statement on The Scope and Appropriate Use of the Term Probiotic." Nature Reviews Gastroenterology & Hepatology. 2014; 11 (8): 506–14
- Patel RM, et al. Therapeutic use of prebiotics, probiotics, and postbiotics to prevent necrotizing enterocolitis: what is the current evidence?. Clin Perinatol. 2013;40(1):11-25.
- Shamir R, et al. Gut Health in Early Life: Significance of the Gut Microbiota and Nutrition for Development and Future Health. 2015; John Wiley and Son.
- Vighi G, et al. Allergy and the Gastrointestinal System. Clinical and Experimental Immunology.2008;153:3-6.
- Tibbs TN, et al. The influence of the microbiota on immune development, chronic inflammation, and cancer in the context of aging. Microbial Cell. 2019;6(8): 324 – 334.
- Harm Wopersis H, et al. The first thousand days – intestinal microbiology of early life: establishing a symbiosis. Pediatr Allergy Immunol. 2014;25(5):428-38.
- Belkaid Y, et al. Role of the microbiota in immunity and inflammation. Cell. 2014;157(1):121-41.
- O'Hara AM, et al. The gut flora as a forgotten organ. EMBO Rep. 2006;7(7):688-93.
- McDermott AJ, et al. The microbiome and regulation of mucosal immunity. Immunology. 2014;142(1):24-31.
- Belizário JE, et al. Microbiome and Gut Dysbiosis. Exp Suppl. 2018;109:459-476.
- DeGruttola AK, et al. Current Understanding of Dysbiosis in Disease in Human and Animal Models. Inflamm Bowel Dis. 2016;22(5):1137-50.
- Carding S, et al. Dysbiosis of gut microbiota in disease. Microb Ecol Health Dis. 2015;V26:26191
- Hawrelak JA, et al. The causes of intestinal dysbiosis: a review. Altern Med Rev. 2004;9(2):180-197
- Lee YY, et al. Gut microbiota in early life and its influence on health and disease: A position paper by the Malaysian Working Group on Gastrointestinal Health. J Paediatr Child Health. 2017;53(12):1152-1158.
- Prescott SL, et al. Early-life environmental determinants of allergic diseases and the wider pandemic of inflammatory noncommunicable diseases. J Allergy Clin Immunol. 2013;131(1):23-30
- Moossavi S, et al. The Prebiotic and Probiotic Properties of Human Milk: Implications for Infant Immune Development and Pediatric Asthma. Front Pediatr. 2018 Jul 24;6:197.
- Jeurink PV et al. Human milk: a source of more life than we imagine. Benef Microbes. 2013;4(1):17-30.
- Corona L, et al. Human Milk Oligosaccharides: A Comprehensive Review towards Metabolomics. Children (Basel). 2021 Sep 14;8(9):804.
- Dong P, et al. Early-life gut microbiome and cow's milk allergy- a prospective case - control 6-month follow-up study. Saudi J Biol Sci. 2018;25(5):875-880.
- Candy D, et al. A synbiotic-containing amino-acid-based formula improves gut microbiota in non-IgE-mediated allergic infants. Pediatr Res. 2018; 83:677–686.
- Liu Y,et al. Modulation of Gut Microbiota and Immune System by Probiotics, Pre-biotics, and Post-biotics. Front Nutr. 2022;8:634897.
- Sorensen K, et al. The Use of an Amino Acid Formula Containing Synbiotics in Infants with Cow’s Milk Protein Allergy—Effect on Clinical Outcomes. Nutrients. 2021;13: 2205.
- NICE. Cow’s milk allergy in children. [internet] [updated 2023 June; cited 2023 June 12]. Available from: https://cks.nice.org.uk/topics/cows-milk-allergy-in-children/#:~:text=Cow%27s%20milk%20allergy%20is%20a,more%20proteins%20in%20cow%27s%20milk
- Luyt D, et al. BSACI guideline for the diagnosis and management of cow's milk allergy. Clin Exp Allergy. 2014;44(5):642-672.
- NHS. What should I do if I think my baby is allergic or intolerant to cow’s milk? [internet] [updated 2022 November 28; cited 2023 January 27]. Available from: https://www.nhs.uk/common-health-questions/childrens-health/what-should-i-do-if-i-think-my-baby-is-allergic-or-intolerant-to-cows-milk/
- Hubbard G, et al. Synbiotic containing extensively hydrolyzed formula improves gastrointestinal and atopic symptom severity, growth, caregiver quality of life, and hospital-related healthcare use in infants with cow's milk allergy. Immune inflame & Dis. 2022;10(6):e636.
* SYNEO synbiotic blend: Bifidobacterium breve M-16V (probiotic) & short and long-chain galacto- and/or fructo-oligosaccharides (prebiotic). The only synbiotic blend within hypoallergenic formulas in the UK.'
† Market comparison of UK EHF and AAF data cards, September 2023.
Help us provide information most relevant to you
Please ensure your role and areas of interest are up to date.